We're all clear (I hope) on the principle that MTs--at least in the US--do not diagnose or prescribe. It would be a massive overreach to do so, and we'd deserve the smackdown that would result if we got caught doing it.
It would never be right for us to inform someone that they have a particular disease, nor to prescribe to them what they should do about any condition they have.
But we do observe during a session, and as a result, we sometimes see things that need to have prompt action taken, in order to protect the client from harm.
So we need to be skillful about reporting what we observe to the client--we may need to balance the urgency of making it clear to the client how serious it is to follow up, versus not diagnosis, prescribing, or unnecessarily frightening them.
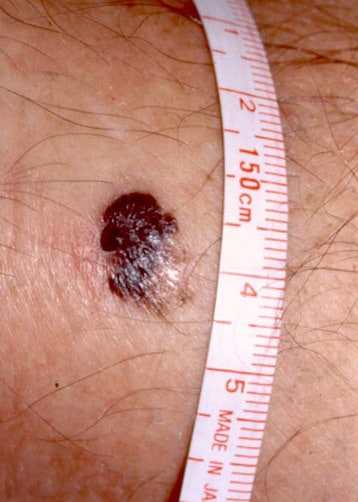
There are many anecdotal cases of MTs telling clients that they should get a suspicious skin lesion checked out. When the diagnosis turns out to be melanoma, which--if it remained undetected--would very likely disfigure and then kill them, then the MT rightly gets the credit for saving the client's life.
Source: http://img.medscape.com/pi/emed/ckb/dermatology/1048885-1100753-2560.jpg accessed 20 August 2012
Melanoma accounts for only 4% of all skin cancers; however, it causes the greatest number of skin cancer–related deaths worldwide. Early detection of thin cutaneous melanoma is the best means of reducing mortality.--Medscape, "Cutaneous Melanoma" accessed 20 August 2012
Sometimes, that early detection that is the best means of reducing mortality (the death rate) comes from an MT who observes something, and tells the client "I think you ought to get that checked out with your primary healthcare provider.".
This case report is similar, yet the lesion the MT observed and recommended follow-up for to the client came from a very different condition.
Syphilis is a horrible way to die.

Source: "Portrait of Gerard de Lairesse by Rembrandt van Rijn, circa 1665–67, oil on canvas - De Lairesse, himself a painter and art theorist, suffered from congenital syphilis that severely deformed his face and eventually blinded him." http://upload.wikimedia.org/wikipedia/commons/4/42/Rembrandt_Harmensz._van_Rijn_095.jpg accessed 20 August 2012
The man in this picture was born with ("congenital") syphilis, and you can see, even in a painting, how disfigured his face is from the disease.
The bacteria that cause syphilis, Trepomena pallidum, are spirochetes--spiral-shaped--as you can see in this electron micrograph from Wikipedia, and are spread mainly by direct sexual contact, and also from mother to child at birth:

Source: http://upload.wikimedia.org/wikipedia/commons/2/29/Treponema_pallidum.jpg accessed 20 August 2012
Although syphilis is referred to as "protean" (versatile, flexible, changeable) in the article we're about to review, because it can take so many forms, there is a typical presentation that's considered classic of the disease:
- Stage I--Primary syphilis: A chancre (painless sore). Usually occurs about 3 weeks after initial exposure to infection.
- Stage II--Secondary syphilis: Widespread rash, often involving hands and feet, possibly including other symptoms of infection such as fever, headache, weight loss. Usually occurs about 4-10 weeks after Stage I.
- Stage III--Latent syphilis: Asymptomatic. Usually occurs around a year after initial infection.
- Stage IV--Tertiary syphilis: Ulcerated lesions, neurological symptoms (loss of balance, apathy, seizures, dementia), cardiac symptoms (inflammation of aorta, aneurysms). Usually occurs anywhere from 3 to 45 years after initial infection.
The disease has been recorded in art and literature in Europe since about the 1500s. That fact, and the discovery of thousand-year-old tombs in Peru, where mummies and bones showed signs of the disease, reinforce the hypothesis that the disease originated in the New World, and was brought back to Europe by the crews of explorers and conquerors.

Source: http://images.nationalgeographic.com/wpf/media-live/photos/000/542/cache/peru-tomb-80-individuals-found-skeleton_54286_600x450.jpg accessed 21 August 2012
Syphilis goes back in recorded history for centuries--most of that time without effective treatment--and devastated people of all classes and walks of life. Those facts, along with the intimate linkage of the disease with love and sex, means that it figures largely in literature and art of the 18th and 19th centuries.
Keats' poem, "La Belle Dame Sans Merci (The Beautiful Lady Without Pity)" is often interpreted to represent the disease as a beautiful lover, who coldly strikes down kings, princes, and knights with no regard for their suffering:
I met a lady in the meads,
Full beautiful—a faery’s child,
Her hair was long, her foot was light,
And her eyes were wild....
I made a garland for her head,
And bracelets too, and fragrant zone;
She look’d at me as she did love,
And made sweet moan....
She found me roots of relish sweet,
And honey wild, and manna dew,
And sure in language strange she said—
“I love thee true.”She took me to her elfin grot,
And there she wept, and sigh’d fill sore,
And there I shut her wild wild eyes
With kisses four....
I saw pale kings and princes too,
Pale warriors, death-pale were they all;
They cried—“La Belle Dame sans Merci
Hath thee in thrall!”--John Keats, "La Belle Dame Sans Merci (The Beautiful Lady Without Pity)", 1884 accessed 21 August 2012
Twentieth-century medicine--specifically, the discovery of the antibiotic penicillin--made enormous inroads into the suffering caused by syphilis, and in the developed world, the disease is much more under control than it used to be. (It's a different story in the developing world, and that's a big enough topic to deserve its own post later on.)
But cases still occur, and although it's unlikely that you'll ever have a client suffering from untreated syphilis, it's not totally impossible, either.
Here's a case report of an MT who observed something suspicious, acted upon that suspicion, and probably saved the client's life, sparing him a great deal of suffering from the later stages of the disease, as well.
Case report:
Introduction
Syphilis is a disease with protean manifestations that often goes undetected in its early stages. Recently an upsurge in syphilis has been reported amongst gay men in various parts of the UK despite changes in sexual behaviour towards safer sex as a consequence of the HIV epidemic. We report a case of syphilis in which transmission occurred despite safer sex in which the diagnosis was flagged up by the observations of a complementary therapist.
Important take-home points:
- Syphilis is "protean"--changeable, variable, flexible. It can take many forms.
- Because it can be so changeable, its early stages--where it's most treatable--can go undetected. If the disease is missed in the early stages, that lays the groundwork for the devastating later stages that can include neurosyphilis and cardiac involvement.
- The HIV epidemic has led to safer sex practices, which is turn had led to a decrease in syphilis rates, BUT recently (2003, as of this article) syphilis rates have surged higher--why this is the case, they do not say.
- The MT was the one who observed the symptoms of syphilis in this client and referred him for diagnosis and treatment of what turned out to be a very serious disease.
Case report
A 50-year-old HIV-positive gay man attended a complementary therapist on the infectious diseases ward for a massage in July 2001.
Here's an example of where massage is incorporated into a hospital ward in a National Health Service (NHS) hospital in England.
We know the client is HIV-positive, so opportunistic infections--ones that take the opportunity of establishing themselves, with the immune system weakened by HIV--are always something to keep in mind as a risk for this client.
The masseuse noticed a rash on the patient’s feet that was not present on previous visits and referred him directly to the HIV clinic the same day.
Important take-home points:
- Although the rash on the feet is part of the classic symptomatic presentation in Stage II syphilis, there are many other things it could be as well, and we never diagnose.
- The MT referred the client directly to the HIV clinic (where there are primary healthcare providers to diagnose and treat), where he was seen the same day.
Without diagnosing, and without panicking the client, what might you say to get the client to follow up with their primary healthcare provider in a case like this?
If you think about what you might say, and rehearse it, then--if you ever need it--you won't be struggling to come up with words on the spot.
Six weeks previously he had noticed an infection around the nail on his left middle finger which had responded only partially to antibiotics from his general practitioner. He was otherwise well with an undetectable viral load, CD4 count of 640 cells/mL and was taking trizivir and efavirenz as antiretroviral therapy.
Again, we don't diagnose, and would never say so to the client--but it's pretty clear that that was the classic Stage I chancre (painless sore) presentation of syphilis.
It is interesting that it responded only partially to antibiotics from the GP. Did the GP miss anything? Would we comment on that to the client?
Figure 1. "Paronychia of middle finger—site of primary chancre" accessed 20 August 2012
He had a long-term male partner with whom he practised oral sex only. Six weeks previously he had contact with a casual male partner in a sauna in London where he had practised active digital rectal penetration but did not have penile penetrative anal sex.
Would we ever ask for this information in an intake or history?
Might this information ever come to us in a different way? If so, in what ways?
What would we do with this information?
If we have a problem with this behavior, would we tell the client?
What is the ethical way for a healthcare provider to deal with aspects of a client's sexual history that might make us uncomfortable?
On examination, he had a maculopapular rash over his trunk and the soles of his feet. A soft tissue swelling was apparent around the nail of his left middle finger, which was not ulcerated and resembled a paronychia (Figure 1). General examination was otherwise unremarkable.
Although the article did not include a picture of the client's rash, this is an example from Wikipedia of what a secondary syphilitic rash can look like:

Source: http://upload.wikimedia.org/wikipedia/commons/e/eb/2ndsyphil2.jpg accessed 21 August 2012
He underwent a sexual health screen, including urethral, pharyngeal and rectal swabs and syphilis serology. All results were negative except syphilis serology which showed: rapid plasma reagin test: positive 1:64, Treponema pallidum particle agglutination assay: positive, > 1280, syphilis IgM enzyme-linked immunosorbent assay (ELISA) positive, Syphilis IgG ELISA Positive.
Important take-home points:
- His bloodwork tested negative for everything else, and positive for syphilis.
He was reviewed five days later with the results of these tests. The rash over his trunk had increased and he had developed painful papules over the palms of his hands. The apparent paronychia on his left middle finger remained. A diagnosis of secondary syphilis was made and he received an uneventful 14-day course of procaine penicillin 600,000 U by intramuscular injection. His regular partner received a full sexual health screen that was negative. The casual sexual contact was untraceable.
Discussion
The case is of interest for a number of aspects. It is probable that this patient’s primary chancre was the lesion noted on his left middle finger. Syphilitic chancres involving the hand with a paronychia have been reported but are uncommon[1,2]. Since the decline of syphilis in the 1980s there are no reports of syphilitic paronychias. This man developed syphilis despite practising 'safer sex'. Recently there has been an increase in syphilis in gay men in the UK. Most cases appear to be acquired from casual sexual contacts in meeting places where anonymity is a feature.
This is the sentence that stands out the most for me in this article, as it shows what real and important value our observations can provide to the client:
The abnormal rash was identified initially by a complementary practitioner who advised that a medical opinion be sought without delay.
The rest of the article is a summation of the situation at the time the article was written:
The Public Health Laboratory Service reports that the number of cases of syphilis in the UK has increased over the last 2 years[3]. In 2000 there were 321 cases of syphilis in England and Wales, and between 1998-2000 an increase of 191% was observed in males. A greater proportion of syphilis infections are transmitted amongst men who have sex with men than any other sexually transmitted infection. The risk of HIV transmission in gay men is also increased when a syphilis infection is present. Since 1997, there have been a number of outbreaks of syphilis in major cities, including Manchester and Brighton. In Manchester nearly half the cases diagnosed were in HIV-positive gay men[4].
Oral sex is quoted as an important factor in the transmission of syphilis in these outbreaks, although our case report highlights another potentially high-risk sexual practice. Whilst the risk of transmission of syphilis can be minimized by using a condom for oral and anal sex, other sexual practices perceived as low risk may still carry a risk of infection.
And, once again, the MT's role in observing something unusual and referring the client to a primary healthcare provider is re-emphasized:
The case also reinforces the need for all staff working within the field of HIV/genitourinary medicine and indeed, other health care professionals, to be vigilant for clinical signs in patients who otherwise appear asymptomatic. In this case it was the masseuse not the clinicians who identified the abnormal rash of secondary syphilis.
The importance of the MT's action should not be underestimated. We've seen what effects undetected and untreated syphilis can have over the course of decades.
By getting the client diagnosed and treated, the MT took action that probably saved the client years of suffering, followed by a dismal death.
References
- Kingsbury DH, Chester EC, Jansen GT. Syphilitic paronychia: an unusual complaint. Arch Dermatol 1972;105:458.
- Starzychi Z. Primary syphilis of the fingers. Br J Vener Dis 1983;59:169-71.
- Fenton KA, Nicoll A, Kinghorn G. Resurgence of syphilis in England: time for more radical and nationally coordinated approaches. Sex Trans Inf 2001;77:309-10.
- Lacey HB, Higgins SP, Graham D. An outbreak of early syphilis: cases from North Manchester General Hospital. Sex Transm Infect 2001;77:311-13.